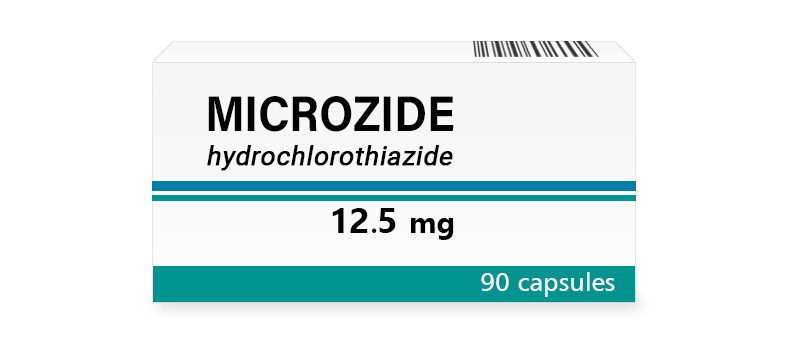
Microzide 12.5 mg Capsules
Hydrochlorothiazide at the base of Microzide helps to get rid of excess water. The drug lowers blood pressure and eliminates swelling associated with the heart or kidneys. Its action is mild but steady, which is convenient for daily monitoring. It is used for conditions with fluid retention.
| Dosage | Package | Per Item | Per Pack | Order |
12.5 mg |
|
The brand version of Microzide is not available without a prescription in your region and requires a doctor’s consultation and approval.
Brand Name
This medication is marketed under the trade name Microzide, widely acknowledged among healthcare practitioners for its effectiveness in managing fluid retention and blood pressure.
International Nonproprietary Name (INN)
The active ingredient is universally recognized as hydrochlorothiazide, ensuring its consistent identification across global medical frameworks.
Form of Release
The drug is presented as capsules, designed for oral intake and available in specific strengths to meet diverse therapeutic needs. These capsules are crafted for ease of administration and maintain stability under standard storage conditions.
Composition
Hydrochlorothiazide constitutes the core active component, engineered to influence fluid balance and vascular dynamics within the body. Supporting this are auxiliary substances such as lactose monohydrate, corn starch, magnesium stearate, and gelatin, which form the capsule structure and aid in its disintegration upon ingestion. Some formulations may include colorants like titanium dioxide or iron oxide to distinguish strengths visually. Each element is purposefully integrated to enhance the therapeutic impact of hydrochlorothiazide while preserving its reliability.
Pharmacologic Properties
Pharmacodynamics
This medication functions as a thiazide diuretic, targeting the distal convoluted tubule in the kidneys to exert its effects. It inhibits the sodium-chloride symporter, increasing the excretion of sodium, chloride, and water, which reduces plasma volume and subsequently lowers blood pressure. This action also promotes potassium loss, though to a lesser extent than loop diuretics, and indirectly enhances calcium reabsorption. Beyond fluid reduction, it contributes to vasodilation over time, further supporting its antihypertensive properties. Effects typically begin within two hours of administration, peaking at three to six hours, with benefits sustained through regular use. Its mechanism provides a balanced approach to managing conditions involving excess fluid or elevated vascular pressure.
Pharmacokinetics
Upon oral consumption, the drug absorbs efficiently from the gastrointestinal tract, achieving a bioavailability of approximately 60% to 80%, with minimal impact from food intake. Peak plasma concentrations are reached within one to two hours. Hydrochlorothiazide binds moderately to plasma proteins, around 40% to 68%, and remains largely confined to the extracellular space, with limited tissue penetration. It undergoes negligible hepatic metabolism, being excreted primarily unchanged through urine via glomerular filtration and tubular secretion. Elimination accounts for about 95% of the dose within 24 hours, with a half-life ranging from 5 to 15 hours, depending on renal function. Conditions impairing kidney performance can prolong this duration, necessitating careful monitoring.
Indications for Use
This medication is recommended for conditions requiring fluid and pressure regulation. It is primarily employed to manage hypertension, effectively reducing elevated blood pressure through its diuretic action, suitable for mild to moderate cases. It also addresses edema associated with congestive heart failure, liver cirrhosis, or nephrotic syndrome, alleviating fluid buildup in tissues and reducing cardiac workload. In certain instances, it supports treatment of edema linked to corticosteroid or estrogen therapy. Additionally, it may be used to prevent kidney stone formation in patients with high urinary calcium levels by enhancing calcium retention. Its broad utility makes it a key option for both standalone and combination therapy in these scenarios.
Contraindications
Specific health conditions restrict the use of this drug to ensure patient safety. Sensitivity to hydrochlorothiazide, sulfonamide-derived compounds, or capsule ingredients prohibits its administration, as reactions could range from mild rashes to severe allergic episodes. Complete absence of urine production or severe renal impairment with creatinine clearance below 30 mL/min renders it unsuitable due to its reliance on kidney excretion. Significant liver dysfunction, particularly with risk of hepatic coma, excludes its use because of potential electrolyte disturbances. It is avoided in cases of uncorrected severe electrolyte imbalances, such as low potassium or sodium, to prevent further disruption. Known hypersensitivity to sulfonamides or a history of acute gout flares also contraindicates it, given its potential to elevate uric acid.
Method of Administration and Dosage
How to Take
Capsules are taken orally, preferably in the morning to minimize nighttime urination, and can be consumed with or without meals. Swallowing them whole with water ensures proper delivery to the digestive system. Maintaining a consistent schedule each day supports steady therapeutic levels for effective management.
Dosage for Adults and Children
For adults managing hypertension, treatment typically starts at 12.5 mg once daily, with adjustments to 25 mg or 50 mg daily based on pressure response. For edema, 25 mg to 100 mg daily is common, divided into one or two doses depending on fluid reduction needs, with a maximum of 200 mg in severe cases. Pediatric dosing begins at 1 mg to 2 mg per kilogram daily, split into two doses, with a maximum of 37.5 mg per day for infants up to 2 years and 100 mg for older children, tailored under expert guidance. Regular monitoring ensures both efficacy and safety across age groups.
Dose Adjustment in Specific Conditions
Renal impairment requires cautious use; doses may remain at 12.5 mg daily if clearance is 30 to 60 mL/min, but it’s avoided below 30 mL/min due to reduced excretion capacity. Mild liver issues suggest maintaining lower doses, such as 12.5 mg daily, with close tracking of electrolyte levels, though severe dysfunction typically rules out its use. Older adults or those with compromised fluid status may start at 12.5 mg daily to reduce risks of low pressure or electrolyte shifts. Frequent evaluations confirm that dosing aligns with each patient’s physiological needs, particularly in vulnerable states.
Side Effects
This medication may elicit a variety of unintended responses, most of which are mild and manageable. Dizziness or lightheadedness often occurs, typically linked to blood pressure reductions, especially during initial use or dose increases. Fatigue, muscle cramps, or weakness might arise, frequently tied to electrolyte changes like low potassium or magnesium. Dry mouth or increased thirst can signal mild dehydration, addressable with adequate fluid intake. Gastrointestinal discomfort, such as nausea or upset stomach, affects some individuals but usually resolves over time. Rarely, serious reactions like significant electrolyte imbalance—potentially causing heart irregularities—or hypersensitivity responses such as rash or jaundice emerge, necessitating immediate medical attention. Periodic blood tests help detect and address these effects early.
Overdose
Symptoms of Overdose
Excessive intake can lead to pronounced hypotension, resulting in dizziness, fainting, or circulatory collapse due to excessive fluid loss. Electrolyte imbalances, such as critically low potassium or sodium, might cause muscle weakness, spasms, or irregular heartbeats, posing risks if uncorrected. Nausea, lethargy, or confusion could indicate systemic disruption, while severe dehydration might escalate to drowsiness or seizures in extreme cases. These symptoms typically appear within hours and intensify without intervention, reflecting the drug’s strong diuretic influence.
First Aid Measures
In an overdose scenario, discontinue administration immediately and seek urgent medical assistance. If taken recently, activated charcoal may limit absorption, applied under professional supervision. Intravenous fluids restore hydration and pressure, while electrolyte corrections address imbalances like potassium or sodium deficits. Monitoring heart rhythm and kidney function stabilizes the patient until recovery, focusing on swiftly reversing overdose effects. Supportive care ensures circulatory and metabolic stability is regained.
Drug Interactions
Effects on Other Medications
This drug can influence the performance of other medications when used together. It may enhance the pressure-lowering effects of additional antihypertensive agents, requiring dose adjustments to avoid excessive declines. Pain relievers like ibuprofen might reduce its fluid-reducing capacity, adding kidney strain over time. Lithium levels could rise due to decreased clearance, necessitating blood monitoring. It might amplify the glucose-lowering effects of diabetes medications, risking low blood sugar, so regular checks are advised. Medications affecting heart rhythm, such as some antiarrhythmics, could increase irregularity risks, needing electrocardiogram oversight. Careful management minimizes these interaction concerns.
Compatibility with Alcohol and Food
Alcohol intake may heighten fluid loss or low pressure, increasing dizziness risks, so moderation is recommended. Meals do not significantly alter absorption, allowing flexible timing, though high-sodium diets might counteract fluid reduction, suggesting dietary balance. Potassium-rich foods like bananas can help offset potassium loss but should be monitored to prevent excess.
Special Precautions
Use During Pregnancy and Breastfeeding
This medication is generally avoided during pregnancy unless benefits outweigh potential downsides, as it may cross the placenta and affect fetal fluid balance or growth, based on limited evidence. It appears in breast milk in small amounts, potentially altering infant electrolyte levels, so nursing mothers should consult their physician, possibly opting for alternatives to minimize exposure.
Impact on Driving and Machinery Operation
Dizziness or tiredness, especially when beginning or adjusting doses, could impair driving or machinery operation. Patients should assess their tolerance before such activities, ensuring safety for themselves and others.
Considerations for Elderly and Pediatric Populations
Older adults may need lower initial doses due to age-related declines in kidney function or fluid reserves, with monitoring for pressure drops or electrolyte changes. In children, its use is tailored to specific needs, with weight-based doses adjusted cautiously under expert guidance to avoid developmental effects. Personalized approaches optimize outcomes across these groups.