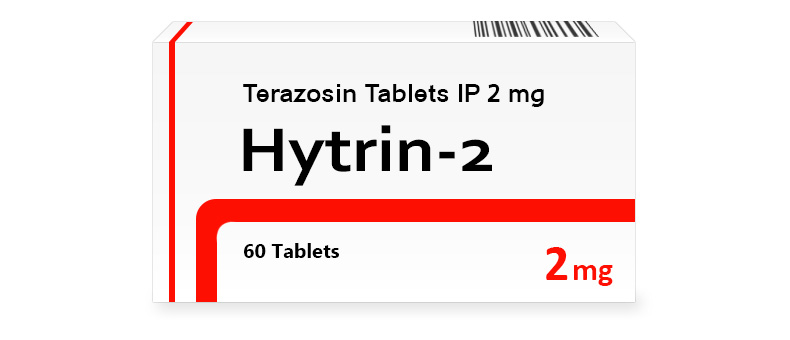
Hytrin 2 mg Tablets
Terazosin in Hytrin dilates blood vessels and facilitates urination. It is effective in hypertension and enlarged prostate, reducing pressure and improving urine flow. Its action relaxes the muscles, which helps with two problems at once. It is used for those who are facing similar disorders.
| Dosage | Package | Per Item | Per Pack | Order |
2 mg |
|
The brand version of Hytrin is not available without a prescription in your region and requires a doctor’s consultation and approval.
Brand Name
This medication is available under the trade name Hytrin, a name widely recognized in medical circles for addressing specific health issues.
International Nonproprietary Name (INN)
The active ingredient is known globally as terazosin, ensuring uniform identification across healthcare systems.
Form of Release
The drug is offered as tablets, formulated for oral use with various strengths to suit diverse patient needs. These tablets are designed for convenience and stability under typical conditions.
Composition
Terazosin hydrochloride serves as the primary active component, engineered to target particular bodily processes. Supporting ingredients include lactose monohydrate, corn starch, pregelatinized starch, and magnesium stearate, which maintain tablet structure and aid dissolution. A coloring agent may differentiate strengths visually. These elements enhance terazosin’s therapeutic action without affecting its potency.
Pharmacologic Properties
Pharmacodynamics
This medication acts as an alpha-1 adrenergic receptor antagonist, targeting smooth muscle receptors to achieve its effects. It blocks norepinephrine’s vasoconstrictive action, relaxing blood vessel walls and reducing peripheral resistance. This lowers blood pressure, making it useful for hypertension. It also relaxes prostate and bladder neck muscles, improving urine flow in benign prostatic hyperplasia. Effects start within hours, peaking over days to weeks with regular use. Terazosin’s selective action limits interference with other receptors, ensuring targeted efficacy.
Pharmacokinetics
After oral administration, the drug absorbs well from the digestive tract, with bioavailability near 90%, largely unaffected by meals. Terazosin peaks in plasma within one to two hours. It undergoes extensive liver metabolism via glucuronidation and hydrolysis, forming inactive metabolites. It distributes broadly, binding about 90% to plasma proteins, reaching vascular smooth muscle and prostate tissues. Elimination is mainly through bile and feces, with around 40% exiting in urine as metabolites. The half-life ranges from 9 to 12 hours, possibly lengthening with liver or kidney issues, needing dose adjustments. Steady levels establish within days of consistent dosing.
Indications for Use
The medication treats conditions needing vascular or urinary management. It effectively reduces high blood pressure by lowering vascular tone, aiding hypertension control. It’s also used for symptomatic benign prostatic hyperplasia, easing urinary obstruction and enhancing flow by relaxing key muscles. In some cases, it may assist kidney stone passage by relaxing ureteral smooth muscle off-label. Its dual role in cardiovascular and urological care makes it versatile, often part of broader treatment plans.
Contraindications
Certain conditions restrict the use of this drug to avoid serious risks. Hypersensitivity to terazosin or quinazoline derivatives prohibits it, as reactions might range from skin issues to anaphylaxis. Severe low blood pressure or past orthostatic collapse rules it out due to its pressure-lowering effects. Significant liver impairment contraindicates it, as slowed metabolism risks buildup. Combining it with phosphodiesterase-5 inhibitors like sildenafil needs careful oversight to avoid worsened hypotension. Severe dehydration or volume loss requires correction first to prevent circulatory issues.
Method of Administration and Dosage
How to Take
Tablets are taken orally, often at bedtime to lessen initial dizziness, with or without food. Swallowing them whole with water ensures proper delivery. A regular schedule maintains steady levels.
Dosage for Adults and Children
Adults with hypertension typically start at 1 mg daily, rising to 2 mg, 5 mg, or 10 mg daily based on response, up to 20 mg in some cases. For benign prostatic hyperplasia, 1 mg at bedtime begins treatment, titrated to 5 mg or 10 mg daily for symptom relief. Pediatric use lacks firm guidelines, but when prescribed, dosing starts at 0.5 mg daily, adjusted cautiously under expert care. Pressure and symptom checks guide increments for safety and efficacy.
Dose Adjustment in Specific Conditions
Renal impairment usually needs no change, as little is excreted unchanged in urine, though fluid status monitoring is wise. Liver dysfunction suggests lower doses, like 1 mg daily, due to slower metabolism and buildup risks. Elderly or low-pressure patients may also start lower to avoid excessive hypotension or orthostatic effects. Regular checks ensure dosing fits individual needs.
Side Effects
The medication may cause various unintended effects, differing in frequency. Dizziness or lightheadedness, often from postural pressure drops, is common, especially after initial or increased doses. Fatigue, headaches, or drowsiness might occur, usually fading with time. Nasal congestion or palpitations can stem from vasodilation. Fluid retention or leg swelling is less common but noted. Rare severe issues, like syncope—brief unconsciousness—or priapism in men, need urgent care. Patient input and check-ups manage these effectively.
Overdose
Symptoms of Overdose
Taking too much can cause severe hypotension, leading to dizziness, fainting, or circulatory collapse from excessive vessel relaxation. Tachycardia might arise to compensate, though shock could follow in extreme cases. Weakness, confusion, or lethargy may accompany these, showing significant pressure drops. Symptoms emerge within hours and worsen without care, reflecting strong vascular impact.
First Aid Measures
Stop the drug immediately in an overdose and seek urgent medical help. Recent ingestion may call for gastric lavage or charcoal under supervision to limit uptake. IV fluids or vasopressors like norepinephrine can treat low pressure, with monitoring to stabilize heart rate and pressure. Lying flat with legs raised may help initially until aid arrives. Focus is on restoring circulation quickly.
Drug Interactions
Effects on Other Medications
This drug alters other medications’ effects when combined. It may boost antihypertensive actions, risking steep pressure drops, needing dose tweaks. With phosphodiesterase-5 inhibitors, it heightens hypotension risks, requiring spacing or oversight. Beta-blockers might worsen orthostatic effects, needing slow titration. It may also lessen vasoconstrictors like phenylephrine’s impact by opposing them. Adjustments and monitoring reduce these risks.
Compatibility with Alcohol and Food
Alcohol might worsen hypotension or dizziness with the medication, especially from added vasodilation, so moderation is wise. Food doesn’t notably affect uptake, allowing flexible timing, though low-salt diets support pressure benefits. No specific food limits apply beyond balance.
Special Precautions
Use During Pregnancy and Breastfeeding
The drug isn’t advised in pregnancy unless benefits outweigh risks, as animal data suggest fetal harm, though human evidence is scarce. It may enter breast milk minimally, so nursing mothers should consult their doctor, possibly choosing alternatives to limit infant exposure.
Impact on Driving and Machinery Operation
Dizziness or drowsiness, especially at start or dose shifts, may hinder driving or machinery use. Patients should test their response before such tasks, ensuring safety.
Considerations for Elderly and Pediatric Populations
Older adults might need lower initial doses due to greater sensitivity to pressure drops, with tolerance checks. In children, use is rare and specialist-managed, with weight-based dosing monitored for developmental effects. Tailored care optimizes safety and results.