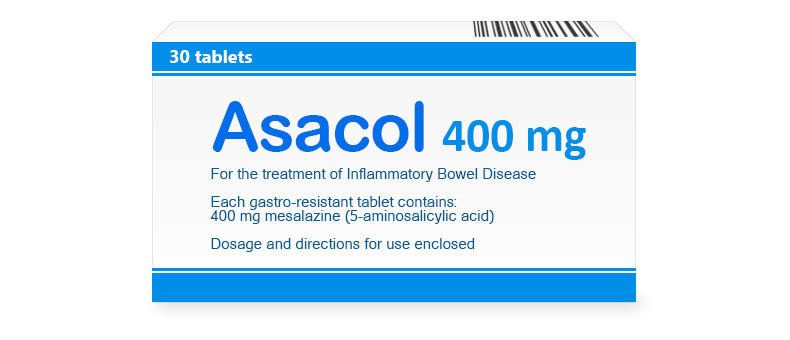
Asacol 400 mg Tablets
Mesalamine, the base of Asacol, reduces inflammation in the intestines. It is effective in ulcerative colitis and Crohn's disease by protecting the mucosa from damage. It acts locally, relieving pain and abdominal cramps. It is used by people with chronic digestive problems.
| Dosage | Package | Per Item | Per Pack | Order |
400 mg |
|
The brand version of Asacol is not available without a prescription in your region and requires a doctor’s consultation and approval.
Brand Name
The medication is marketed under the brand name Asacol, a widely recognized label in the field of gastrointestinal inflammatory disorder management.
International Nonproprietary Name (INN)
The active ingredient in this product is identified globally as mesalamine, a name standardized for consistency across international pharmacological practices.
Form of Release
Asacol is available as delayed-release oral tablets, designed to deliver the active substance to the lower gastrointestinal tract. These tablets come in strengths of 400 mg and 800 mg, typically packaged in bottles or blister packs to support precise dosing and storage.
Composition
Each delayed-release tablet of Asacol contains mesalamine as the primary active substance, with dosages of 400 mg or 800 mg. The formulation includes several inactive ingredients, such as microcrystalline cellulose, which provides structural support, and sodium starch glycolate, aiding in disintegration. Additional excipients like magnesium stearate act as lubricants, while the enteric coating comprises methacrylic acid copolymer, dibutyl phthalate, and iron oxides to ensure release in the colon. Trace stabilizers maintain the drug’s stability, ensuring reliable efficacy throughout its shelf life.
Pharmacologic Properties
Pharmacodynamics
Asacol functions as an anti-inflammatory agent, exerting its effects locally in the gastrointestinal mucosa. It inhibits the production of pro-inflammatory mediators, such as prostaglandins and leukotrienes, by blocking cyclooxygenase (COX) and 5-lipoxygenase pathways in colonic epithelial cells. This reduction in inflammation alleviates symptoms like abdominal pain, diarrhea, and rectal bleeding in inflammatory bowel diseases. Its action is primarily topical, targeting the inflamed mucosa rather than systemic pathways, which minimizes widespread effects.
The medication also modulates cytokine release and scavenges free radicals, further reducing tissue damage and promoting mucosal healing. Clinical studies demonstrate its ability to induce remission in 40–70% of mild to moderate ulcerative colitis cases within 6–8 weeks, with sustained benefits in maintenance therapy. It does not alter systemic immune function significantly, focusing on localized control. This targeted mechanism underpins its efficacy in managing chronic intestinal inflammation.
Pharmacokinetics
Following oral administration, Asacol releases mesalamine in the terminal ileum and colon due to its pH-dependent enteric coating, with minimal absorption in the stomach or proximal small intestine. Systemic bioavailability is low, around 20–30%, as most of the dose acts locally, with peak plasma concentrations reached within 4 to 7 hours. The drug binds to plasma proteins at approximately 43%, distributing mainly to the gastrointestinal tract.
Metabolism occurs in the liver and intestinal mucosa via N-acetylation, forming N-acetyl-5-aminosalicylic acid, an inactive metabolite. The half-life ranges from 0.5 to 1.5 hours for mesalamine, with the metabolite persisting up to 7 hours. Elimination is predominantly fecal, with 50–70% excreted unchanged or as metabolites in stool, and 20–30% in urine, reflecting its localized action and minimal systemic clearance.
Indications for Use
Asacol is prescribed for the treatment of mild to moderate ulcerative colitis in adults, where it induces remission by reducing inflammation and associated symptoms like diarrhea and bleeding. It is also indicated for maintenance therapy in ulcerative colitis to prevent flare-ups, offering long-term disease control. The medication addresses distal colitis, including proctitis, targeting inflammation in the lower colon and rectum.
In some cases, it may be used off-label for Crohn’s colitis with predominant colonic involvement, though efficacy varies. It suits patients requiring localized anti-inflammatory action without systemic immunosuppression. These applications highlight its role as a key therapy in managing inflammatory bowel diseases effectively.
Contraindications
Asacol is contraindicated in patients with known hypersensitivity to mesalamine, salicylates, or any tablet component, such as dibutyl phthalate, where reactions could range from rash to anaphylaxis. It is also prohibited in those with severe renal impairment (creatinine clearance below 30 mL/min) due to potential toxicity from metabolite accumulation.
Use is restricted in patients with active peptic ulcer disease, as it may exacerbate gastric irritation, though this is rare with enteric coating. Severe liver dysfunction warrants caution, and the medication should not be used in those with a history of mesalamine-induced pericarditis or myocarditis. Children under 5 or those with aspirin sensitivity syndromes are excluded due to safety concerns.
Method of Administration and Dosage
Administration Guidelines
The tablets should be taken orally, swallowed whole with water, with or without food, as the enteric coating ensures colonic release regardless of meal timing. They should not be chewed, crushed, or split, as this disrupts the delayed-release mechanism and reduces efficacy. Consistent daily timing supports steady therapeutic levels.
Dosage for Adults and Children
For adults with active ulcerative colitis, the typical dose of Asacol is 2.4 g to 4.8 g daily (6–12 tablets of 400 mg or 3–6 of 800 mg), divided into 2–3 doses for 6 weeks. Maintenance therapy uses 1.6 g to 2.4 g daily (4–6 tablets of 400 mg or 2–3 of 800 mg) in divided doses. Children aged 5–17 with body weight over 24 kg receive 36–71 mg/kg daily, up to 4.8 g, divided into 2 doses for active disease, and 1.6–2.4 g daily for maintenance, adjusted by weight. Younger children under 5 lack established dosing.
Dose Adjustment in Specific Conditions
In mild to moderate renal impairment (creatinine clearance 30–60 mL/min), standard doses are used with monitoring, while severe impairment contraindicates use. Mild to moderate liver dysfunction allows normal dosing, but severe cases require caution due to potential metabolite effects. Elderly patients or those with mild symptoms may start at lower doses (e.g., 1.6 g daily), guided by response. Treatment duration aligns with disease activity, avoiding unnecessary prolongation.
Side Effects
Asacol may cause a variety of side effects, though many patients experience only mild reactions with short-term use. Common issues include headache, abdominal pain, or diarrhea, often reflecting disease activity rather than drug effects. Nausea, flatulence, or fatigue are also reported, typically resolving without intervention.
Less frequent effects include rash, dizziness, or joint pain, linked to systemic exposure. Rare but serious reactions, such as acute intolerance syndrome (e.g., cramping, bloody diarrhea), nephrotoxicity, or hypersensitivity pneumonitis, require immediate cessation and medical attention, particularly with prolonged use. Pancreatitis or elevated liver enzymes occur infrequently. Regular monitoring helps distinguish drug-related effects from disease progression.
Overdose
Symptoms of Overdose
Excessive intake of Asacol may amplify typical side effects, such as nausea, vomiting, or abdominal discomfort, with rare reports of tinnitus or confusion resembling salicylate toxicity. Doses exceeding 10 g daily have shown no consistent severe pattern, reflecting its low systemic absorption.
First Aid Measures
In case of overdose, medical consultation is advised, though emergency measures are rarely needed. No specific antidote exists, so treatment focuses on supportive care, such as hydration for gastrointestinal upset or rest for fatigue. Monitoring renal function and symptoms is recommended until resolution, typically within 24–48 hours, given the drug’s clearance profile.
Drug Interactions
Effects on Other Medications
Asacol has minimal systemic interactions due to its local action, but co-use with nephrotoxic drugs like NSAIDs or tacrolimus may increase renal risk, requiring monitoring. It may reduce azathioprine or 6-mercaptopurine efficacy by interfering with their metabolism, potentially necessitating dose adjustments. Antacids or laxatives altering intestinal pH could affect the enteric coating, though this is uncommon.
Drugs like warfarin or digoxin show no significant interaction, as mesalamine does not affect cytochrome P450 enzymes. Patients should report all medications to their healthcare provider to manage these minor interactions effectively.
Compatibility with Alcohol and Food
Moderate alcohol use does not directly impair efficacy but may worsen colitis symptoms, suggesting limited intake during therapy. Food does not affect release or absorption significantly, allowing flexible administration with or without meals for patient convenience.
Special Precautions
Use During Pregnancy and Breastfeeding
Asacol is Category B in pregnancy, with no clear fetal harm in limited data, used cautiously if benefits outweigh risks. It passes into breast milk in small amounts, primarily as the metabolite, so breastfeeding is generally safe with monitoring for infant diarrhea, guided by medical advice.
Women of childbearing age should confirm non-pregnant status before starting high doses and discuss risks with their provider during therapy.
Impact on Driving and Operating Machinery
The medication may cause dizziness or fatigue in some patients, suggesting caution with driving or machinery until tolerance is clear. Most individuals resume normal activities once adjusted, but initial use warrants observation for these effects.
Considerations for Elderly and Pediatric Populations
Elderly patients tolerate Asacol well, with no significant efficacy differences, though renal function monitoring is key due to age-related decline. Children aged 5–17 with ulcerative colitis can use weight-based dosing, while those under 5 lack established safety data, limiting use to older pediatric groups.